Cancer mortality rates fall across Canada, but progress stalls on cervical cancer
Open this photo in gallery:
Cervical cancer screening rates plummeted during the worst of the COVID-19 pandemic, fewer people have a family doctor to remind them when they’re due for a Pap or HPV test, and screening may simply not be top of mind for women in early middle age.ETHAN CAIRNS/The Canadian Press
Cancer mortality rates continue to fall in Canada, driven by decreases in the death rates from lung and colorectal cancer, but progress has stalled against one type of cancer that is entirely preventable.
Cervical cancer rates have plateaued, according to a major report on cancer trends published every two years by Statistics Canada, the Public Health Agency of Canada and the Canadian Cancer Society.
The latest edition, released Monday, found that the long-running decline in cervical cancer incidence rates – a measure of newly diagnosed cases – has levelled off when women of all ages are considered. The same is true of death rates.
However, incidence rates are actually rising among women aged 35 to 54, according to Darren Brenner, a cancer epidemiologist and co-chair of the Canadian Cancer Statistics Advisory Committee.
“Back in the 1950s, death rates from cervical cancer were about six times higher than they are today,” said Dr. Brenner, also a professor in the departments of oncology and community health sciences at the University of Calgary. “For the first time, these rates are no longer decreasing, and this is concerning, given that we’ve been talking about the potential elimination of cervical cancer.”
Cervical cancer is almost always caused by the sexually transmitted human papillomavirus, or HPV. HPV infection is preventable with a vaccine that is usually offered in middle school, but the shot wasn’t approved for use in Canada until 2006 and uptake varies across the country.
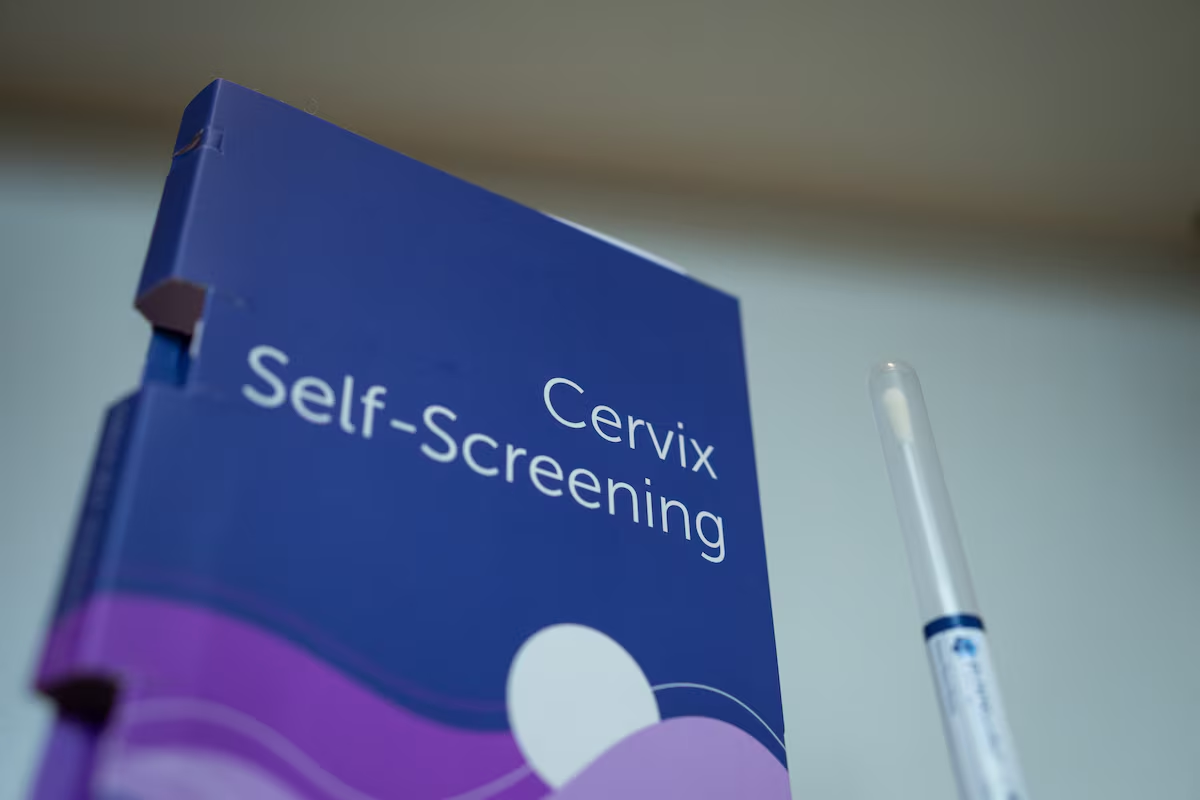
The disease can also be prevented through screening with the Pap test or a newer test that detects infection with cancer-causing strains of HPV. Precancerous cervical lesions caught through screening can be removed, stopping cancer before it starts.
Canada has committed to eliminating cervical cancer by 2040.
“What we know from this report is that Canada is not on track to meet that goal,” said Brandon Purcell, the manager of advocacy for the Canadian Cancer Society.
There are several theories for why fewer women are getting screened for cervical cancer today than in the past, according to Dr. Brenner. Screening rates plummeted during the worst of the COVID-19 pandemic, fewer people have a family doctor to remind them when they’re due for a Pap or HPV test, and screening may simply not be top of mind for women in early middle age.
“These are very busy periods of people’s lives,” Dr. Brenner said.
Shannon Pethick knows firsthand the consequences of putting off screening for cervical cancer. She was diagnosed with stage 2b cervical cancer in 2010 at the age of 32.
Radiation and chemotherapy saved her life, but left her unable to have children. Now 47 and working in finance in Saskatoon, she still feels a pang of sadness when Mother’s Day comes around every year.
“I was very much, like, oh, it doesn’t matter. Let’s put it off. I’ll deal with it later,” Ms. Pethick said of cervical cancer screening. “Being on the other side of that now, there’s too much at stake to let it go.”
The discouraging news on cervical cancer doesn’t undermine the good news in other realms of cancer.
The mortality rates for lung, bladder and colorectal cancers have been falling by more than 3 per cent a year, the report found – although lung cancer still kills more Canadians than any other kind.
“The preventive focus on reducing commercial tobacco use in Canada, we’re starting to see that impact in lung cancer incidence, and similarly in lung cancer mortality,” said Jennifer Gillis, director of surveillance for the Canadian Cancer Society.
The reduction in bladder cancer mortality rates is also owing mostly to fewer people smoking. Cigarettes are a leading cause of bladder cancer.
When it comes to colorectal cancer, screening with stool tests, starting in much of Canada about a decade ago, followed by colonoscopies, has allowed more patients to have precancerous cells removed, preventing cancer.
However, well-organized government screening programs for colorectal cancer are generally aimed at people 50 and older, so younger Canadians aren’t reaping the benefits of early detection.
Colorectal cancer rates have been rising in Canadians younger than 50, which “may reflect increases in poor diet, sedentary lifestyle and obesity rates in post-baby boomer generations,” according to the report.
Some of the same factors could be behind a small increase in breast-cancer rates among younger women, the report found. It noted that breast-cancer rates in Canada have risen by 0.2 per cent a year since 2006, but the increase is steeper among women in their 20s, 30s and 40s.
However, the breast-cancer mortality rate fell by 1.5 per cent between 2011 and 2022, mostly owing to improved access to mammograms and better treatments.
Despite falling incidence and mortality rates in some cancers, more individual Canadians get cancer every year. That is because the population is growing and aging. Cancer risk rises with age.
An estimated 254,800 Canadians are projected to be diagnosed with cancer this year, and 87,400 are expected to die of it. Cancer remains the leading cause of death in Canada.
Editor’s note: This article has been updated to correct the title of Brandon Purcell, advocacy manager of prevention and early detection with the Canadian Cancer Society.